Search
- Page Path
- HOME > Search
Original Article
- Bone Metabolism
- Comparison of the Effects of Various Antidiabetic Medication on Bone Mineral Density in Patients with Type 2 Diabetes Mellitus
- Jeonghoon Ha, Yejee Lim, Mee Kyoung Kim, Hyuk-Sang Kwon, Ki-Ho Song, Seung Hyun Ko, Moo Il Kang, Sung Dae Moon, Ki-Hyun Baek
- Endocrinol Metab. 2021;36(4):895-903. Published online August 9, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1026
- 6,159 View
- 230 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Prospective comparative studies on the effects of various antidiabetic agents on bone metabolism are limited. This study aimed to assess changes in bone mass and biochemical bone markers in postmenopausal patients with type 2 diabetes mellitus (T2DM).
Methods
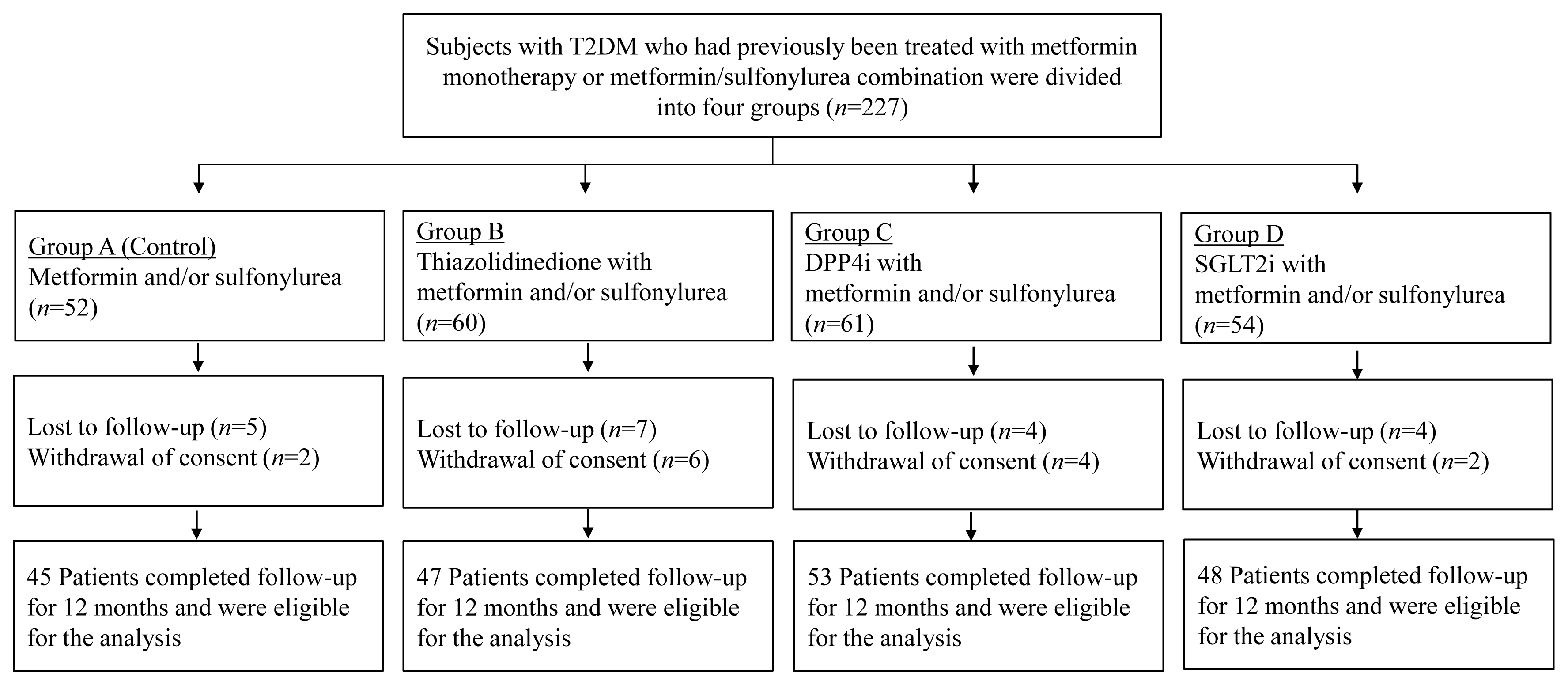
This prospective, multicenter, open-label, comparative trial included 264 patients with T2DM. Patients who had received a metformin, or sulfonylurea/metformin combination (Group 1); a thiazolidinedione combination (Group 2); a dipeptidyl peptidase-4 inhibitor (gemigliptin) combination (Group 3); or an sodium-glucose cotransporter 2 inhibitor (empagliflozin) combination (Group 4) were prospectively treated for 12 months; bone mineral density (BMD) and bone turnover marker (BTM) changes were evaluated.
Results
The femoral neck BMD percentage changes were −0.79%±2.86% (Group 1), −2.50%±3.08% (Group 2), −1.05%±2.74% (Group 3), and −1.24%±2.91% (Group 4) (P<0.05). The total hip BMD percentage changes were −0.57%±1.79% (Group 1), −1.74%±1.48% (Group 2), −0.75%±1.87% (Group 3), and −1.27%±1.72% (Group 4) (P<0.05). Mean serum BTM (C-terminal type 1 collagen telopeptide and procollagen type 1 amino-terminal propeptide) levels measured during the study period did not change over time or differ between groups.
Conclusion
Significant bone loss in the femoral neck and total hip was associated with thiazolidinedione combination regimens. However, bone loss was not significantly associated with combination regimens including gemigliptin or empagliflozin. Caution should be exercised during treatment with antidiabetic medications that adversely affect the bone in patients with diabetes at a high risk of bone loss. -
Citations
Citations to this article as recorded by- Meta-Analysis on the Association Between DPP-4 Inhibitors and Bone Mineral Density and Osteoporosis
Lili Huang, Wei Zhong, Xinghuan Liang, Huijuan Wang, Shi-en Fu, Zuojie Luo
Journal of Clinical Densitometry.2024; 27(1): 101455. CrossRef - A multicentre, double‐blind, placebo‐controlled, randomized, parallel comparison, phase 3 trial to evaluate the efficacy and safety of pioglitazone add‐on therapy in type 2 diabetic patients treated with metformin and dapagliflozin
Soo Lim, Seung‐Hwan Lee, Kyung‐Wan Min, Chang Beom Lee, Sang Yong Kim, Hye Jin Yoo, Nan Hee Kim, Jae Hyeon Kim, Seungjoon Oh, Jong Chul Won, Hyuk Sang Kwon, Mi Kyung Kim, Jung Hwan Park, In‐Kyung Jeong, Sungrae Kim
Diabetes, Obesity and Metabolism.2024;[Epub] CrossRef - Association of Bone Turnover Markers with Type 2 Diabetes Mellitus and Microvascular Complications: A Matched Case-Control Study
Yilin Hou, Xiaoyu Hou, Qian Nie, Qiuyang Xia, Rui Hu, Xiaoyue Yang, Guangyao Song, Luping Ren
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 1177. CrossRef - Complementary effects of dapagliflozin and lobeglitazone on metabolism in a diet-induced obese mouse model
Yun Kyung Lee, Tae Jung Oh, Ji In Lee, Bo Yoon Choi, Hyen Chung Cho, Hak Chul Jang, Sung Hee Choi
European Journal of Pharmacology.2023; 957: 175946. CrossRef
- Meta-Analysis on the Association Between DPP-4 Inhibitors and Bone Mineral Density and Osteoporosis

Case Reports
- A Case of Incidentally Diagnosed Adrenal Paragonimiasis.
- Shin Ae Park, Seung Hwan Lee, Seung Hyun Ko, Jun Gi Kim, Soo Youn Park, Jin Young Yoo, Ho Woo Nam, Yu Bae Ahn
- Endocrinol Metab. 2011;26(1):97-100. Published online March 1, 2011
- DOI: https://doi.org/10.3803/EnM.2011.26.1.97
- 1,853 View
- 23 Download
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - We report here on a rare case of adrenal paragonimiasis that presented with an adrenal incidentaloma. A 52-year-old male presented with fatigue and weight loss. The laboratory findings revealed eosinophilia (8.5%) and an increased eosinophil count (910/microL). The computed tomography scan showed 6.5 x 5 cm sized multilocular cystic mass in the right adrenal gland, which was non-functioning, and cystic lesions with variable sizes were also noted in the abdominal cavity. On the surgical field, whitish patches were spread out in the peritoneum, the omentum, the dome of the liver and the diaphragm. The right adrenal gland was replaced by a cystic mass filled with mucopurulent creamy materials. The pathologic findings revealed numerous eggs of Paragonimus spp. Also, the ELISA was positive for IgG paragonimus antibody. The adrenal gland can become infected by various microbial pathogens, including parasites, although it is relatively uncommon. However, in the case of a cystic adrenal mass with accompanying eosinophilia in an endemic area, clinicians should consider the possibility of parasitic infection.
-
Citations
Citations to this article as recorded by- Paragonimus westermani infection manifesting as a pulmonary cavity and adrenal gland mass: A case report
Yong Shik Kwon, Hye Won Lee, Hyun Jung Kim
Journal of Infection and Chemotherapy.2019; 25(3): 200. CrossRef - A Case of Ectopic Peritoneal Paragonimiasis Mimicking Diverticulitis or Abdominal Abscess
Min Jae Kim, Sung-Han Kim, Sang-Oh Lee, Sang-Ho Choi, Yang Soo Kim, Jun Hee Woo, Yong Sik Yoon, Kyung Won Kim, Jaeeun Cho, Jong-Yil Chai, Yong Pil Chong
The Korean Journal of Parasitology.2017; 55(3): 313. CrossRef - Paragonimiasis in the Abdominal Cavity and Subcutaneous Tissue: Report of 3 Cases
Chang Ho Lee, Jong Hun Kim, Woo Sung Moon, Min Ro Lee
The Korean Journal of Parasitology.2012; 50(4): 345. CrossRef
- Paragonimus westermani infection manifesting as a pulmonary cavity and adrenal gland mass: A case report

- A Case of Ectopic Neurohypophysis Presenting with Hypogonadism.
- In Woon Baek, Ji Hyun Kim, Guk Jin Lee, Kyoung Eun Lee, Hae Lim Lee, Hye Won Lee, Nam Yong Kim, Yon Kwon Ihn, Seung Hyun Ko, Seung Hwan Lee, Je Ho Han
- Endocrinol Metab. 2011;26(1):67-71. Published online March 1, 2011
- DOI: https://doi.org/10.3803/EnM.2011.26.1.67
- 2,216 View
- 27 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - Pituitary stalk interruption and ectopic neurohypophysis seen on magnetic resonance Imaging (MRI) are often associated with either isolated growth hormone (GH) deficiency or combined anterior pituitary hormone deficiency, but their pathogenesis is not clear and the clinical data regarding these anatomical defect is limited. We experienced a 23-year-old male with the absence of secondary sexual characteristics and this was accompanied with pituitary stalk dysgenesis and ectopic neurohypophysis. He received growth hormone for a year when he was 12 years old due to his short stature. Sella MRI showed no visible pituitary stalk with minimal high signal change, suggesting ectopic neurohypophysis. The combined pituitary stimulation test revealed blunted responses of growth hormone, follicle stimulating hormone and luteinizing hormone. For the hypogonadotropic hypogonadism, the patient was given testosterone intramuscularly and he gradually developed secondary sexual characteristics. We concluded that the hypogonadism and growth hormone deficiency in this patient was caused by hypopituitarism due to pituitary stalk dysgenesis and ecopic nuerohypophysis.
-
Citations
Citations to this article as recorded by- MRI of ectopic posterior pituitary gland with dysgenesis of pituitary stalk in a patient with hypogonadotropic hypogonadism
Ashim Kumar Lahiri, Ramanivas Sundareyan, David Jenkins, Anjumara Nilak
Radiology Case Reports.2018; 13(4): 764. CrossRef - Hypothalamic Hypopituitarism Caused by Pituitary Stalk Dysgenesis
Seong-Ju Lee, Hye-Jin Yoon, A-Reum Cho, Yoo-Jin Um, Keun-Young Park, Dong-Mee Lim, Byung-Joon Kim
Korean Journal of Medicine.2013; 85(4): 420. CrossRef
- MRI of ectopic posterior pituitary gland with dysgenesis of pituitary stalk in a patient with hypogonadotropic hypogonadism

- Two Cases of Primary Hyperparathyroidism Associated with Colon Cancer.
- Sang Hoon Chun, Yun Kyung Kim, Jae Seung Yun, Eun Hee Jang, Shin Ae Park, Jae Hyung Cho, Seung Hyun Ko, Yu Bai Ahn, Young Jin Suh, Jun Gi Kim
- J Korean Endocr Soc. 2008;23(3):204-209. Published online June 1, 2008
- DOI: https://doi.org/10.3803/jkes.2008.23.3.204
- 2,308 View
- 45 Download
-
 Abstract
Abstract
 PDF
PDF - Hypercalcemia is often observed in cancer patients secondary to parathyroid hormone (PTH) related peptide production. However, primary hyperparathyroidism and colon cancer rarely present simultaneously. Calcium is believed to have a chemopreventive effect against colorectal cancer because it reduces crypt cell hyperproliferation in both humans and in animals. There is evidence to suggest that the incidence of colorectal cancer in humans is reduced by high calcium intake. In patients with primary hyperparathyroidism, increased PTH activates 1,25(OH)2D and enhances calcium absorption in the gut. Consequently, the calcium level in the lumen is decreased, leading to an elevated risk of colorectal cancer. We report two patients with colon cancer and hypercalcemia secondary to primary hyperparathyroidism, along with a brief review of the literature.

- A Case of Ectopic ACTH Syndrome Associated with Small Cell Lung Cancer Presented with Hypokalemia.
- Hong Jun Yang, Hea Jung Sung, Ji Eun Kim, Hyo Jin Lee, Jin Min Park, Chan Kwon Park, Eun Suk Roh, Jae Hyung Cho, Seung Hyun Ko, Ki Ho Song, Yu Bai Ahn
- J Korean Endocr Soc. 2007;22(5):359-364. Published online October 1, 2007
- DOI: https://doi.org/10.3803/jkes.2007.22.5.359
- 1,953 View
- 26 Download
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF - We report a case of a 73-year-old female patient who was diagnosed with ectopic ACTH syndrome caused by small cell lung cancer. We initially presumed that the patient was in a state of mineralocorticoid excess, because she had hypertension and hypokalemic alkalosis. This was however excluded because her plasma renin activity was not suppressed and her plasma aldosterone/plasma renin activity ratio was below 25. Moreover, her 24 hour urine free cortisol level was elevated and her serum cortisol levels after a low dose dexamethasone suppression test, were not suppressed. Furthermore, her basal plasma ACTH and serum cortisol levels increased and her serum cortisol level after a high dose dexamethasone suppression test was not suppressed. We performed studies to identify the source of ectopic ACTH syndrome and found a 3 cm-sized mass in the patient's right lower lobe of her lung, which was eventually diagnosed as small cell lung cancer following a bronchoscopic biopsy. In conclusion, Cushing's syndrome, and in particular ectopic ACTH syndrome, must be considered in the differential diagnosis of mineralocorticoid-induced hypertension. The excessive cortisol saturates the 11beta-hydroxysteroid dehydrogenase type 2 (11beta-HSD2) activity, which in turn, inactivates the conversion of cortisol to cortisone in the renal tubules. Moreover, excessive cortisol causes binding to the mineralocorticoid receptors, causing mineralocorticoid hypertension, characterized by severe hypercortisolism.
-
Citations
Citations to this article as recorded by- Emergencia hipertensiva como debut de síndrome de Cushing paraneoplásico
E. Rubio González, M. de Valdenebro Recio, M.I. Galán Fernández
Hipertensión y Riesgo Vascular.2024; 41(2): 135. CrossRef - Management of small cell lung cancer complicated with paraneoplastic Cushing’s syndrome: a systematic literature review
Yanlong Li, Caiyu Li, Xiangjun Qi, Ling Yu, Lizhu Lin
Frontiers in Endocrinology.2023;[Epub] CrossRef - Ectopic Cushing Syndrome in Adenocarcinoma of the Lung: Case Report and Literature Review
Rana Al-Zakhari, Safa Aljammali, Basma Ataallah, Svetoslav Bardarov, Philip Otterbeck
Cureus.2021;[Epub] CrossRef - A Case of Ectopic Adrenocorticotropic Hormone Syndrome in Small Cell Lung Cancer
Chaiho Jeong, Jinhee Lee, Seongyul Ryu, Hwa Young Lee, Ah Young Shin, Ju Sang Kim, Joong Hyun Ahn, Hye Seon Kang
Tuberculosis and Respiratory Diseases.2015; 78(4): 436. CrossRef
- Emergencia hipertensiva como debut de síndrome de Cushing paraneoplásico

- A Case of Antineutrophil Cytoplasmic Antibody (ANCA) Positive, Propylthiouracil-Induced Diffuse Alveolar Hemorrhage in Graves' Disease.
- Der Sheng Sun, Dong Kyu Kim, Hyo Jin Lee, Hee Yun Lee, Dae Jun Kim, Eun Sook Kim, Jae Hyoung Cho, Seung Hyun Ko, Wan Ook Kim, Chi Hong Kim, Ki Ho Song, Yu Bae Ahn
- J Korean Endocr Soc. 2007;22(3):215-219. Published online June 1, 2007
- DOI: https://doi.org/10.3803/jkes.2007.22.3.215
- 1,801 View
- 21 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Graves' disease is one of the common autoimmune diseases, and it has been controlled by such antithyroid drugs as propylthiouracil (PTU) or methimazole. There are a number of side effects, including agranulocytosis, skin rash, hepatotoxicity, fever, arthralgia and a lupus-like syndrome during treatment. PTU has been recently observed to be associated with the development of antineutrophil cytoplasmic antibody (ANCA) positive vasculitis, and this can cause diffuse alveolar hemorrhage. A 32-year-old woman with Graves' disease had been treated with PTU for 4 years, and she had experienced intermittent hemoptysis for 2 weeks before she visited the hospital. Both myeloperoxidase and proteinase 3 ANCA were positive without other organ systems being involved. She was diagnosed with PTU-induced vasculitis. Cessation of PTU and administration of corticosteroids improved the clinical manifestations.
-
Citations
Citations to this article as recorded by- A Case of Diffuse Alveolar Hemorrhage with Glomerulonephritis after Propylthiouracil Treatment
Ji Hyun Lee, Min Su Kim, Jae Gon Lee, Dae Sik Kim, Hae Jin Yang, Kyung Woo Kang
Tuberculosis and Respiratory Diseases.2012; 72(1): 93. CrossRef
- A Case of Diffuse Alveolar Hemorrhage with Glomerulonephritis after Propylthiouracil Treatment

- A Case of Cushing's Disease with Renal Cell Carcinomaand End-stage Renal Disease.
- Jang Eun Lee, Ik Jun Choi, Young Jai Park, Hyo Jin Lee, Kyoung Hwan Lee, Seung Hyun Ko, Ki Ho Song, Yu Bai Ahn
- J Korean Endocr Soc. 2007;22(1):62-67. Published online February 1, 2007
- DOI: https://doi.org/10.3803/jkes.2007.22.1.62
- 2,030 View
- 24 Download
-
 Abstract
Abstract
 PDF
PDF - Cushing's disease is the most common cause of endogenous Cushing's syndrome caused by the excessive secretion of adrenocorticotropic hormone (ACTH) by pituitary ACTH-secreting tumors. The tumors are usually microadenomas (< 10 mm in diameter). Macroadenomas are rare, and corticotroph hyperplasia and carcinomas are extremely rare. Patients with these tumors exhibit an increase in plasma ACTH and cortisol levels, elevated urinary excretion of cortisol and adrenocortical steroid metabolites, evidence of altered negative feedback of cortisol and disturbances in neuroendocrine regulation. The diagnosis of Cushing's disease can be challenging in patients with renal failure the presence of abnormal plasma cortisol, poor gastrointestinal tract absorption of dexamethasone and altered functioning of the hypophyseal-pituitary-adrenal axis have been reported in end-stage renal disease, and the urinary cortisol increment method is not reliable in these patients. The prevalence of renal cell carcinoma in patients on dialysis is higher than in the general population. We recently treated a patient with Cushing's disease and end-stage renal disease as a result of renal cell carcinoma. The diagnosis was made by laboratory evaluation of plasma and radiological examination. Here we report a case of Cushing's disease with a review of the medical literature.

- A Case of Lymphocytic Hypophysitis Presented with Hypoglycemia after Delivery.
- Jang Myung Son, Seung Hyun Ko, Yu Bae Ahn, Kang Ju, Jeong Rok Lee, Seong Eun Yang, Ki Ho Song, Ho Young Son, Jeong Su Jun
- J Korean Endocr Soc. 2003;18(3):325-331. Published online June 1, 2003
- 1,081 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - Lymphocytic hypophysitis, an inflammatory disease of the pituitary gland that is often associated with pregnancy, is caused by autoimmune destruction of the pituitary gland evidenced by diffuse inflammatory cell infiltration of the pituitary gland and some kinds of detectable autoantibodies. We report a case of lymphocytic hypophysitis in a 31-year-old woman presenting with severe hypoglycemia and hyponatremia after delivery. Hormonal study revealed panhypopituitarism and magnetic resonance imaging with enhancement showed the bulging contour of the right side pituitary gland with an ill-defined mass-like lesion and nodular thickening of the stalk. The patient's symptoms and biochemical data improved greatly with replacement of L-thyroxine and glucocorticoid. Partial recovery of panhypopituitarism was also seen. The follow-up tests revealed dramatic resolution of the pituitary lesion.

- A Case of Cured Diabetes Mellitus after Pheochromocytoma Removal.
- Chang Kyun Hong, Yu Bae Ahn, Sul Hye Kim, Young Sik Woo, Seoung Goo Lee, Seung Hyun Ko, Ho Ki Song, Kun Ho Yoon, Moo Il Kang, Bong Yeon Cha, Kwang Woo Lee, Ho Young Son, Sung Koo Kang
- J Korean Endocr Soc. 2001;16(4-5):502-507. Published online October 1, 2001
- 1,161 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - Pheochromocytoma is usually associated with a combination of various clinical manifestations caused by the overproduction of catecholamines. It is frequently accompanied by impaired glucose tolerance operating through 2-and-adrenergic mechanisms. A 41-year-old-woman was admitted to the hospital because of poorly-controlled diabetes mellitus and hypertension. She had suffered intermittent paroxysmal attacks of headache and chest discomfort and had been treated intermittently over a 2 year period for diabetes mellitus and hypertension. At admission, the levels of serum epinephrine, norepinephrine urinary excretion of total metanephrine, and VMA were all abnormally elevated. Adrenal CT showed a well-defined, homogenous mass in the right adrenal region and the tumor was diagnosed as pheochromocytoma. After tumor resection, the increased blood level of catecholamines, the urinary excretion of total metanephrine, and VMA were normalized, as was the hyperglycemia state. Diabetes mellitus of the patient was considered permanently resolved after tumor removal by the result of glucose tolerance in 75g oral glucose tolerance test.


 KES
KES

 First
First Prev
Prev



